|
Neurostimulation and intrathecal drug
delivery (IDD) – are indicated to reduce and control
chronic, intractable pain. Which type of therapy to use
can generally be determined by the indication, type of
pain, the pain pattern and the screening period. Studies
have showed that both therapies provide effective pain
relief and significant improvements in quality of life
for people suffering from severe, chronic pain
conditions. In addition, both therapies are reversible
and are preceded by screening tests which help predict
the patients most likely to benefit from treatment.
Both therapies act on specific structures of the nervous
system to reduce and control pain. However, the
mechanism of action and type of pain most responsive to
each therapy differ. Neurostimulation is most effective
for neuropathic pain, while IDD is perceived to be most
effective for nociceptive pain (Table 1). |
|
|
Table 1: Indications and
applications for neurostimulation and
intrathecal drug delivery |
| Neurostimulation |
Intrathecal drug
delivery |
| Neuropathic pain |
● Cancer pain |
| ● Failed back surgery
syndrome (FBSS)* |
● Pancreatitis |
| ● Chronic regional pain
syndromes |
● Spinal cord injury |
| ● Radiculopathy |
● Osteoarthritis |
| ● Diabetic neuropathy |
● Dystonia |
| ● Postherpetic
neuralgia |
● Osteoporosis |
| Peripheral nerve injury |
● Spinal stenosis |
| Ischaemic pain |
● Osteomyelitis |
| ● Peripheral vascular
disease (PVD) |
● Coccygodynia |
| ● Refractory chronic
angina pectoris |
|
| Deafferentation pain |
|
| ● Stump pain |
|
| ● Phantom limb pain |
|
| ● Spinal cord injury |
|
| ● Spinal stenosis |
|
| ● Causalgia |
|
| * Most FBSS
pain comprises a nociceptive as well as a
neuropathic component |
|
. |
|
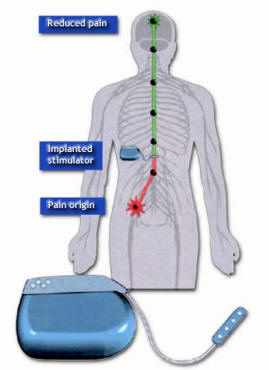
Figure-1: The implanted neurostimulation system |
 |
Patients with chronic
deafferentation or neuropathic pain who are
refractory to previous medical and surgical
therapies may benefit from neurostimulation of
the motor cortex. Motor cortex stimulation
involves implanting an electrode over the motor
cortex region of the brain
corresponding to the area of pain. It is a
reversible procedure and carries less potential
risk to the brain than other surgical
procedures. |
 |
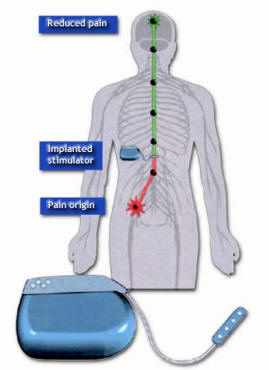
Overview of neurostimulation
Neurostimulation systems use an implanted lead
to deliver low-voltage electrical stimulation to
selected nerves or anatomic structures.
Neurostimulation is divided into subcategories
based upon the type of nerve that is being
stimulated. Spinal cord stimulation (SCS)
involves stimulation of the dorsal column of the
spinal cord by placing electrodes in the space
above the spinal cord. Neurostimulation can also
be used on the peripheral nerves by stimulating
a specific nerve branch in the affected limb.
This site-specific electrical stimulation
inhibits or blocks the sensation of pain in a
targeted region of the body.
In the present document we have focused on the
most frequently used target for neurostimulation
for the treatment of pain. This is often
referred to as ‘spinal cord stimulation’ (SCS)
or ‘stim’. |
 |
The
mechanism of action for neurostimulation
The mechanism of action for neurostimulation is based
upon the use of electricity (Melzack R, Wall PD. Science
1965; 150:971–979). The use of electricity for pain
relief is based on the gate control theory, which
suggests that a metaphorical ‘gate’ exists in the spinal
cord that allows or prohibits the transmission of pain
signals to the brain. |
 |
Neurostimulation systems
Neurostimulation systems consist of three basic
components that generate and deliver electricity in the
form of short bursts or pulses to large nerve fibers in
the dorsal column or the periphery:
● Power source
● Extension
● Surgical or percutaneous leads |
|
 |
create paraesthesia. There are two types of
power sources:
● Internal – Implantable pulse generator
(IPG)
● External – Radio frequency
(RF) system |
 |
Implantable pulse generator (IPG) power source
In an IPG system the entire system, including the
battery, are implanted
within the patient’s body. IPG systems are capable of
meeting the needs of
most patients with chronic pain, except those with very
high expected
energy consumption. For these patients an RF system is
recommended. |
|
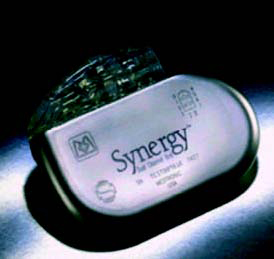
Figure-2: The Synergy Internal (IPG) neurostimulation
system. |
 |
Radio frequency (RF) power source
An RF system consists of two components:
● A transmitter and antenna that are worn externally
● A receiver that is surgically implanted
The external transmitter sends RF signals through the
skin to the implanted
receiver, which is surgically placed under the skin. The
receiver processes
the RF signals from the transmitter and generates
electrical pulses for
neurostimulation. |
 |
Generally patients prefer IPG systems because the
totally implantable IPG
systems are seen as more comfortable, more convenient,
and more
cosmetically appealing than external neurostimulators.
In addition, unlike
RF systems, IPG systems do not cause skin irritations.
For these reasons,
patients will often be more compliant, and overall
therapy will be more
effective. Patients using IPG systems may also have
greater ease in daily
activities, such as working, exercising and sleeping. |
 |
Extension
The extension cable connects the power source to the
lead. Using an
extension rather than a lead connected to the IPG gives
additional benefits
in terms of being easier to handle in case of revisions
and offering more
comfort for patients. |
 |
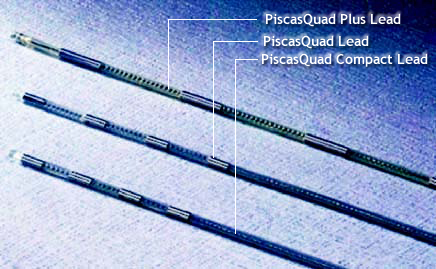
Leads and electrodes
The lead is a polyurethane-encased wire connected to a
set of electrodes.
The lead conducts electrical pulses from the extension
to the electrodes,
which deliver the pulses to large nerve fibers in the
dorsal column or the
periphery. Electrodes are fixed at the end of the lead,
usually in groups of
four. Optimal lead positioning always requires the
cooperation of the
patient and is the key to success with this therapy
(Table 2).
|
|
|
Table 2: Optimal lead positioning |
| Paraesthesia coverage |
Area of stimulation |
| Upper limb |
C3-C5 |
| Precordium |
T1-T2 |
| Lower back and lower
limb |
T8-T9 |
| Foot |
T12-L1 |
|
 |
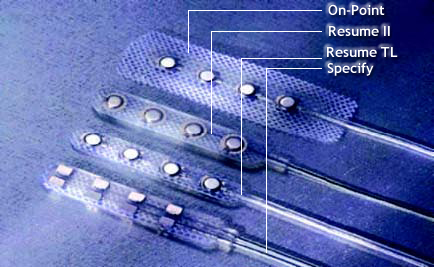
For spinal cord stimulation (SCS), leads are placed in
the epidural space
(between the vertebrae and the dura matter) so that the
electrodes are close
enough to the dorsal horn to stimulate specific large
nerve fibers. Leads can
be implanted into the spinal column in one of two ways
(Table 3):
● Percutaneously through a needle
● Surgically
The functioning neurostimulation
system provides a flow of electrical
pulses from the power source through
the extension and lead to the
electrodes. The electrical pulses are
then conducted into the dorsal column
of the spinal cord or the periphery to
produce paraesthesia. |
|

Figure-3: The Synergy neurostimulator with leads |
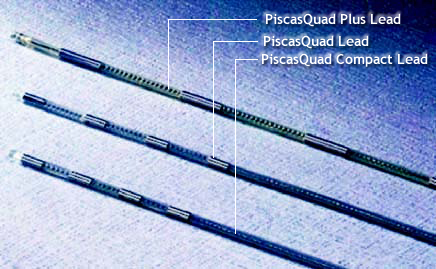
Figure-4: Percutaneous leads |
 |
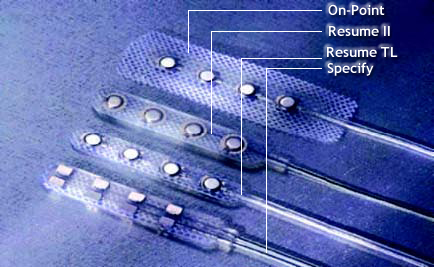
Figure-5: Surgical leads |
|
|
Table 3: Percutaneous and surgical leads |
| |
Percutaneous leads |
Surgical leads |
| Insertion procedure |
● Percutaneous ‘wire’ type
devices can be inserted
via a Tuohy needle |
● Electrodes are
either improved multi-contact versions
of the percutaneous wire type or
plate electrodes requiring
surgical insertion by laminotomy
or partial laminectomy |
| Benefits |
● Often used in
neurostimulation trials because less invasive
than surgical lead implant |
● Enables lead to be securely anchored in place, reducing lead migration both laterally
and longitudinally |
| ● Different
electrode dimensions and spacing |
● Generally accepted that surgical
leads should be used when repeated migrations occur and
when the voltage needed is high
and needs to be reduced |
| ● Surgical implantation with plate
electrodes provide a greater
variety of stimulation patterns
as well as a broader area of
paresthesia |
|
 |
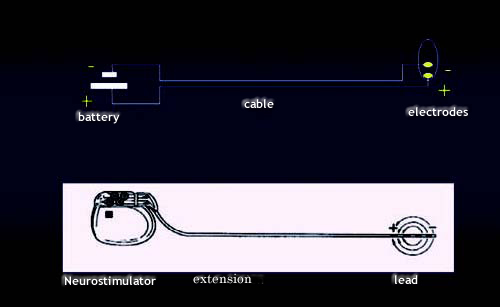
The basic science of neurostimulation
Electricity, which is the flow of electrons from a
negatively charged area or pole, to a positively charged
pole is the key principle of neurostimulation. The
movement of electrons between these two poles is called
an electric current.
Creation of an electrical circuit
An electric current requires a complete electrical
circuit for the electrical
pulses to follow as they travel from the negative to the
positive pole. Three
components are necessary to create a complete electrical
circuit:
● Power source
● Conductor
● Resistance |
|
 |
Because the full
electrical circuit
needs to be
maintained, if there
is no paraesthesia
this could imply that
the circuit is open. |
 |
Power source
The power source provides the source of electrons. The
power source for a
neurostimulation system is the IPG. |
 |
Conductor
A conductor provides the path of least resistance for
the electrical pulses to
move from one pole to another. In a neurostimulation
system, the
conductor comprises of the extension and the lead. |
 |
Resistance – ohms
Resistance, also referred to as impedence, is the
opposition of a material to
an electric current. Resistance is an electrical circuit
that acts to restrict the
flow of electricity through the conductor and is
measured in ohms. The
amount of electric current that travels through a
material depends on the
type of material and its physical dimensions. In a
neurostimulation system,
body tissue and the material from which the leads and
extensions are made
all provide some degree of resistance. Tissue resistance
should normally be
in the range of 50–2000 ohms, with a maximum reading of
4000 ohms. If
the patient is no longer experiencing paraesthesia then
an impedence
measurement test will need to be performed. |
|
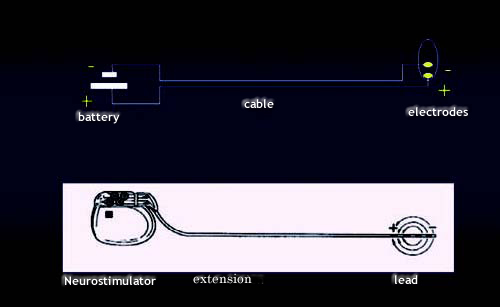
Figure-6: Electric circuit |
 |
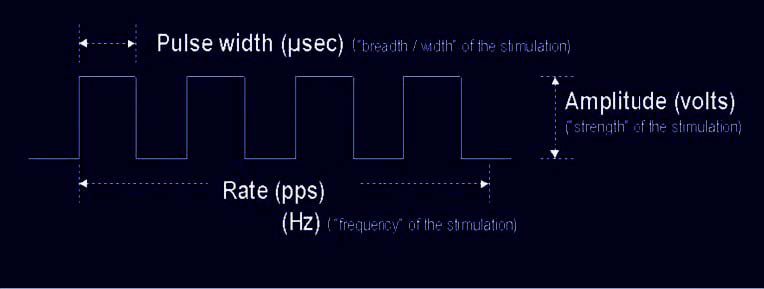
Parameters of an electrical pulse
A neurostimulation system delivers electricity into the
neural targets in the
dorsal column or periphery via electrical pulses
(stimulus) rather than a
continuous electric voltage. Pulses differ from a steady
electric current in
several ways, including:
● The parameters of the pulse
● The way in which the parameters are measured
Electrical pulses are represented by a waveform (Figure
7). A waveform
provides three parameters unique to electrical pulses:
● Amplitude – the strength of the pulse which is
measured in volts (V)
● Pulse width – the length of time that a particular
pulse is delivered
which is measured in microseconds (μs)
● Rate – the number of times per second that a pulse is
delivered which is
measured in pulses per second (pps) or Hertz (Hz) |
 |
Therapeutic parameters
The parameters of a waveform are also the therapeutic
parameters of
neurostimulation and produce the effect of paraesthesia
(Table 4):
● Amplitude – Affects the intensity of the paraesthesia
● Pulse width – Affects the paraesthesia spread or the
patient’s feeling of
paraesthesia
● Rate – Affects the sensation of stimulation
Amplitude, measured in volts (V), affects the intensity
of the paraesthesia. By
increasing the amplitude, the patient will feel the
paraesthesia more strongly.
Paresthesia that is too strong may cause a patient
extreme discomfort or
even pain. Pulse width, measured in microseconds (μs),
affects the lateral
breadth or ‘broadness’ of the paraesthesia. By
increasing the pulse width, the
patient will feel the paraesthesia spread to a larger
area of the painful region.
The third parameter, rate, which is measured in pulses
per second (pps) or
Hertz (Hz), controls the ‘smoothness’ of the
paraesthesia. |
|
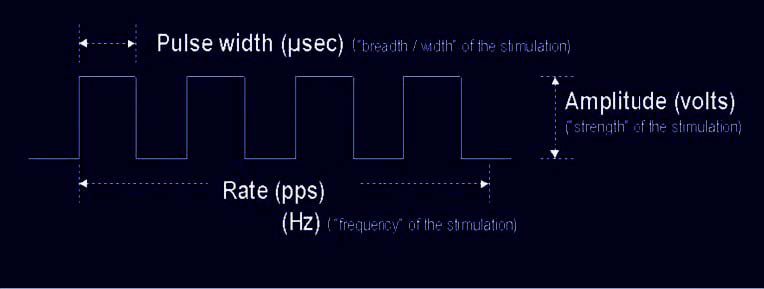
Figure-7: Waveform |
 |
The primary goal of neurostimulation device programming
is to
individualize stimulation parameters to adequately mask
the patient’s
pain pattern, by manipulating the three parameters to
provide the desired
pain relief. |
|
Table 4: Therapeutic parameters of neurostimulation |
| |
Symbol |
Definition |
Therapy affect |
Programming |
| Amplitude |
Volts (V) |
The strength of the
pulse |
Intensity of the
paraesthesia |
Start
at 0 V and increase until paresthesia felt |
| Pulse width |
Microseconds (μs) |
The length of time that
a particular pulse is delivered |
Paraesthesia spread or patient’s feeling of paraesthesia |
Start at
180 μs |
| Rate |
Pulses per
second (pps) or Hertz (Hz) |
The number of times per
second that a pulse is delivered |
Sensation of the
stimulation comfort |
Start at
40 pps and try not to go
over 80pps. If the rate is too low, the patient
will feel a ‘bumpy’
effect. If the rate
is too high, no
additional therapeutic
effect will occur and
the battery will drain
prematurely |
|
 |
Creation of an electric current
A neurostimulation system is programmed for certain
electrodes on the lead
to have a positive charge and other electrodes to have a
negative charge,
producing unipolar or bipolar stimulation. To operate
properly, neurostimulation systems must have at least
one positive electrode(called an anode) and one negative electrode (called a
cathode). |
|
 |
Single-lead stimulation and dual-lead stimulation
Depending on the capabilities of the power source, two
stimulation options
are available:
● Single-lead stimulation
● Dual-lead stimulation |
 |
Single-lead stimulation
Single-lead stimulation is typically
used for patients with simple pain
because the paresthesia generated
by a single lead can effectively mask
the patients pain. In general, single lead
stimulation requires less energy
than dual lead-stimulation.
Some physicians place a single lead
on the midline of the spinal cord in
order to generate paresthesia on
both sides of the body. However,
single-lead systems are not effective in treating
complex pain patterns
because positioning and maintaining a single lead on the
midline of the
spinal cord is often difficult. Furthermore, single-lead
systems do not always
provide adequate paresthesia coverage in complex pain
patterns. |
 |
Dual-lead stimulation
In recent years, dual-lead and dual-channel stimulation
systems such as
Synergy have become available. The dual
stimulation
capability of such devices gives the physician greater
flexibility in managing
hard to treat pain conditions including prominent low
back pain or multiple
pain foci. In particular, dual lead stimulation has
proved to be beneficial for
patients with chronic low back pain and leg pain
associated with failed back
surgery syndrome (FBSS). The great advantage of such a
system is that if
one lead is not sufficient to cover pain adequately a
second one can be
added latter. |
|

Figure-8: Synergy with 1 lead |
| |
|
 |
Advantages of dual-lead stimulation
Dual-lead stimulation systems provide the physician with
more
programming options. This enables them to provide more
effective pain
coverage and therefore greater pain relief. The use of
dual-lead stimulation
systems also enables a reduction in analgesic use.
Depending on the capabilities of the power source,
dual-lead systems can
provide two stimulation modes:
● SingleStim mode
● DualStim mode
Stimulation modes refer to the delivery configuration of
the stimulation
programs. In SingleStim mode, the two leads are
programmed to the same
amplitude, pulse width and rate, thereby producing
stimulation from one
channel. In the DualStim mode, the amplitude and pulse
width can be
programmed in two different ways on both leads providing
stimulation
from two channels. |
|
 The Medtronic Synergy™ neurostimulation
system
The Medtronic Synergy™ neurostimulation
system
Backed by two decades of Medtronic’s experience in implantable
technologies, the Synergy™ system was developed to address the
limitations associated with single-lead neurostimulation systems
and to meet the need for greater flexibility in managing
different types of pain and
laterality of pain. The Synergy™ neurostimulation system is the
first totally implantable dual channel system available for the
management of chronic, intractable pain.
Furthermore, Synergy™ is Medtronic’s most powerful
neurostimulation system, providing greater pain relief for a
longer duration and greater convenience with less frequent
battery replacement. Neurostimulation with Synergy™ increases
the chance of successfully managing more types of pain amongst a
wider range of patients:
● The dual-stimulation capability of Synergy™ confers greater
flexibility, on either one or two leads, to generate
paraesthesia and therefore to provide more effective pain
relief. If one lead is not sufficient to cover pain adequately,
a second lead can be added at a later date
● The use of dual channels, which means that up to 8 electrode
options can be programmed to two independent patterns of
stimulation, enables physicians to cover changing pain patterns
over time
 Components of the Synergy™
neurostimulation system
Components of the Synergy™
neurostimulation system
The Synergy™ system consists of an implantable pulse generator,
an implantable lead (or leads), an extension (or extensions), a
patient programmer and a physician programmer (N’Vision™).
 The Synergy™ implantable pulse generator
The Synergy™ implantable pulse generator
The Synergy™ implantable pulse generator (IPG) generates
electrical impulses to create paraesthesia. The IPG contains a
special battery and electronics to create these impulses. It is
typically implanted under the skin in the abdomen and is
connected to one or two leads which are implanted near the
spinal cord.
 Extensions
Extensions
Medtronic extensions come in a large variety of sizes ranging
from 25–66cm in length. The extension is placed under the skin
and conducts electrical pulses from the implanted Synergy™
neurostimulator to the lead.
 Leads and electrodes
Leads and electrodes
The lead is a special polyurethane-encased wire, available in
lengths of 28cm, 33cm, 45cm and 56cm, which is connected to a
set of electrodes. The lead conducts electrical pulses from the
extension to the electrodes, which deliver the impulses to large
nerve fibers in the dorsal column or the periphery. Electrodes
are fixed at the end of the lead typically in groups of four or
for the octal lead in groups of eight. The Synergy™
neurostimulation system can be used with one lead or two leads,
on one or two channels.
|
Figure 9:The Synergy™ neurostimulation system with leads |
Figure 10 : Synergy™ EZ patient programmer |
 |
 |
 Synergy™ EZ patient programmer
Synergy™ EZ patient programmer
Synergy™ also comes with a patient programmer called Synergy™
EZ. This
is a small, hand-held device that allows patients to make
adjustments to the
neurostimulation parameters within a range set by their
clinician.
Depending on the patient’s need for pain control, patients can
also use this
programmer to turn Synergy™ on and off and to check the battery
status of
the neurostimulator. A 9 V battery is required to operate
Synergy™ EZ.
Synergy™ has been shown to provide effective pain relief
 Results of the Synergy™ system clinical trial, which took place
in nine centers throughout Europe, Australia and Canada and involved 69
patients,
found that patients who were new to treatment and those in whom
other
SCS systems had previously failed responded well to treatment
with
Synergy™. Furthermore, at implantation, mean paraesthesia
coverage was
88.1%, indicating almost complete pain coverage by Synergy™
Results of the Synergy™ system clinical trial, which took place
in nine centers throughout Europe, Australia and Canada and involved 69
patients,
found that patients who were new to treatment and those in whom
other
SCS systems had previously failed responded well to treatment
with
Synergy™. Furthermore, at implantation, mean paraesthesia
coverage was
88.1%, indicating almost complete pain coverage by Synergy™
|
Table 5: Improvement in pain scores with the Synergy™ system
(n=69) |
| |
Patients new to SCS |
Patients switching SCS
to Synergy |
| |
N |
Mean |
N |
Mean |
| Baseline |
39 |
7.53 |
13 |
7.38 |
| Month 3 |
33 |
3.97 |
9 |
5.01 |
| Change |
32 |
3.34 |
9 |
2.77 |
| Baseline vs
Month 3 p-value |
<0.001 |
0.055 |
| Pain was measured using a VAS in 69 patients with chronic pain
treated with the Synergy system |
Neurostimulation with Synergy™ also provided documented patient
satisfaction. At three months, in answer to the question: ‘Based
on your
experience so far, would you have agreed to this stimulation
therapy?’ a
total of 93.6% of patients answered yes. In answer to the
question: ‘Are you
satisfied with the pain relief produced by the Synergy™ system?’
a total of
78.7% of patients answered yes.
Synergy™ has also been shown to significantly improve a
patient’s quality
of life by improving mobility and independence, enabling
patients to
participate in daily activities and return to work, reducing
depression and
improving psychological well-being. |







 What’s Up
What’s Up